Revenue Cycle Management (RCM) Software
Simplify your billing, revenue collection, and insurance claim processing
Book a Demo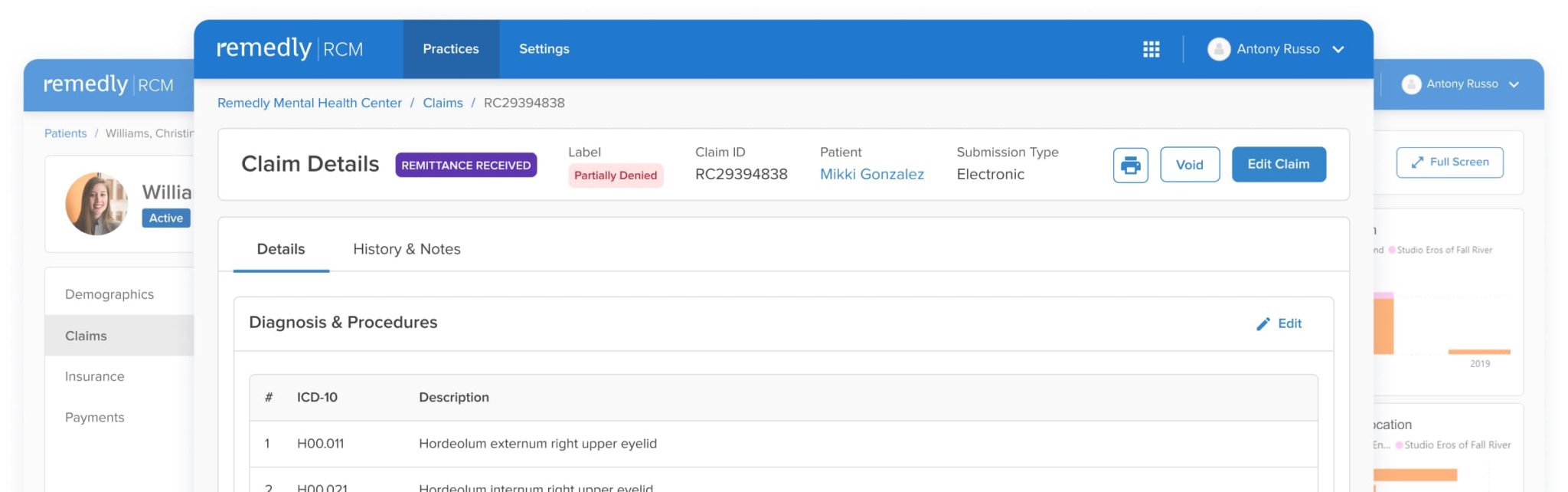

RCM and Medical Billing Features
Revenue Cycle Management has never looked so good. Your Remedly software is a pragmatic solution to manage finances and provide the data you need. Clear and accurate accounts are safely stored for each patient, and patient records can be retrieved easily, equipping you with the ability to make astute decisions. Similarly, ledgers can be viewed for each patient, each company, and each insurance provider as you need. Functionality can be tailored to your practice requirements, but here is a summary of some of our most popular features.
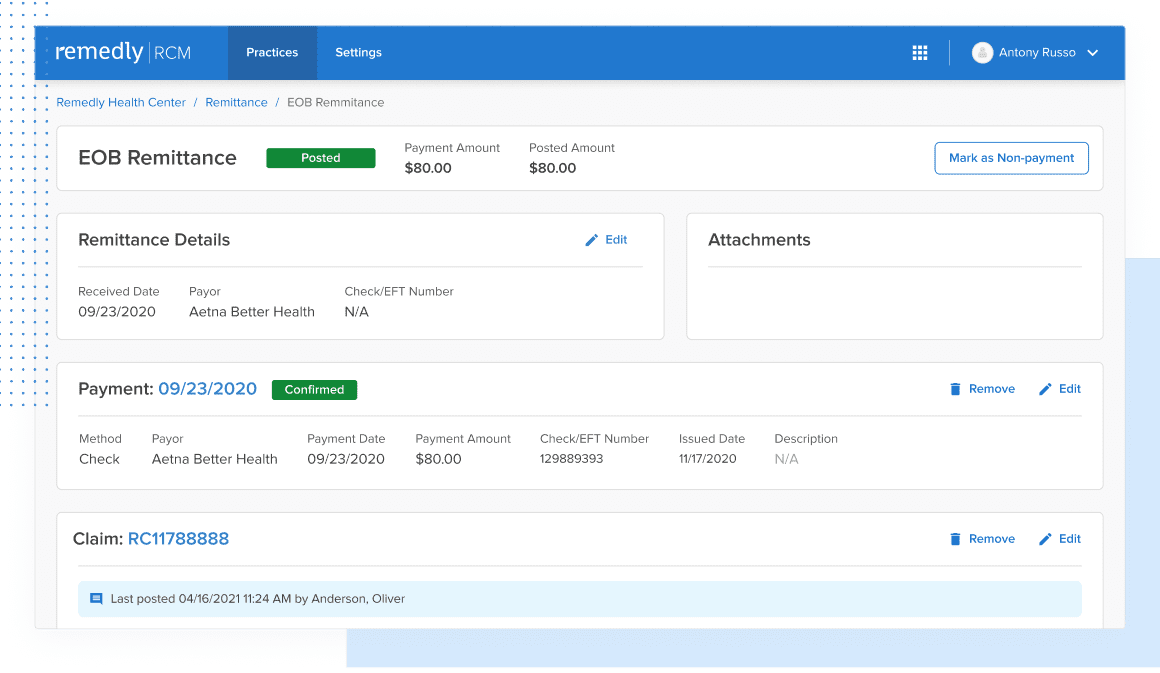
This feature allows a provider to track claim initiation, the response to the claim, and the rationale behind claim denials. Providers can send accompanying notes alongside claims which improve communication, reduce misunderstandings, and minimizes the number of denials. Our claims scrubbing tool keeps the wheels turning to improve your claims acceptance rate. Insurers can respond with notes about the claim, keeping the dialogue open and all parties up-to-speed.
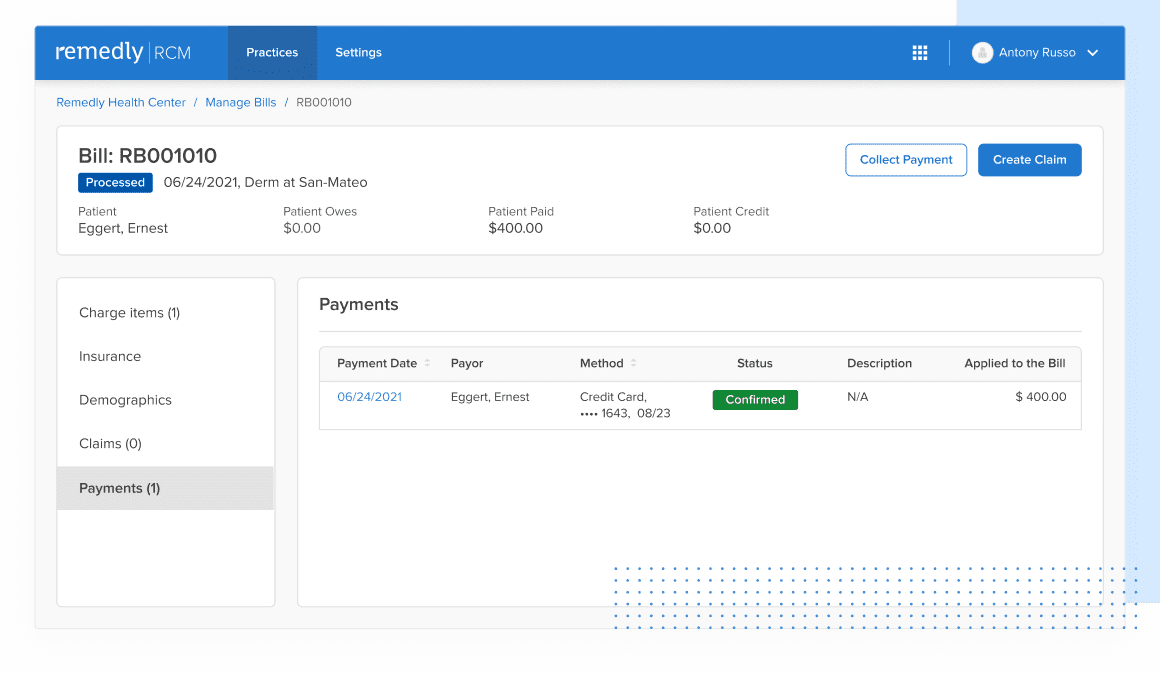
Remedly’s RCM billing software means providers can more easily collect payment from patients with outstanding balances and claim bills from insurers. In addition, our medical billing software logs all of these transactions for historical review.
Remedly’s AI Assistant uses machine learning to predict the acceptance or rejection of claims by clearinghouses and insurance companies before submitting them.
Learn more
Remedly’s medical billing system provides enhanced accuracy of data leading to a decrease in the number of rejected claims and faster revenue collections. Revenue cycle billing also takes care of contract fee schedule management, to ensure you’re receiving maximum claim revenues. Cash flow is more secure, keeping your practice in a strong fiscal position and providing peace of mind. More benefits with Remedly’s revenue cycle management solution include: Contract fee schedule management, Remittance tool, Claims scrubbing
Superbills allow providers to manage bills containing several transactions in a single submission, making it simpler to process the claim. With all the billing in one place, it becomes easier to track, refund, and adjust payments on claims.
To help your practice operate more efficiently, the RCM has built-in integration with different merchant services vendors that will make the process smooth and efficient. In addition, an integrated POS enables patients to pay for services online, save their credit card on file, and keep a record of all transactions in both the EHR and RCM. Additionally, with Remedly’s RCM, you will be able to generate bills and email them to patients for payment with just one click. There are additional benefits to having an integrated POS in terms of business sustainability. You will have more control of inventory and on-site and online sales. Payments can be made via a wide range of payment methods and data is highly secure. Reporting features will enable you to see data including item sales volume, employee sales figures and overall performance. This capability takes the guesswork out of running any business. Knowledge is power, and Remedly’s revenue cycle billing system is knowledge at your fingertips.
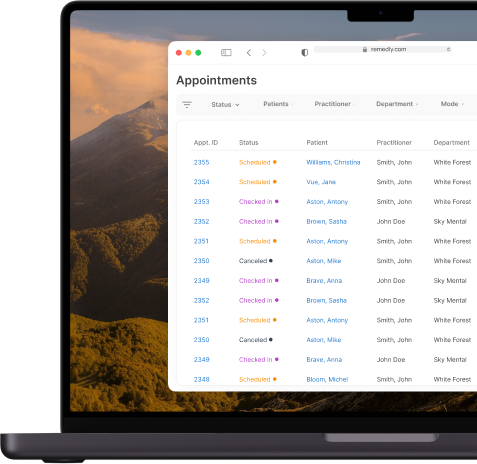
Sifting through data to search for specific information is challenging and time consuming. Remedly’s powerful filters allow you to switch settings easily to take you straight to the information you need. Our electronic medical billing software allows you to work with numerous claims and superbills. Claims can be submitted on paper or electronically. You will also be able to draft appeals and attach relevant files. Providers can track claim initiation, responses to claims, and causes of claim denials. This extremely useful feature helps to keep track of all your claims, keeping you and your patients informed and aware.
Remedly has worked collaboratively with practices to ensure that our revenue cycle management solution provides the reports you need to grow your practice. Our RCM service comes with built-in reporting to produce a depth of analytics. Standard reports include A/R (Accounts Receivable) report for a comprehensive view of outstanding patient billing; summary reports of claims submitted, insurance payments, and payments by encounter as well as payor or service code, among others. Reporting is key and empowers you with the information you need to run an efficient and sustainable practice.

Want to see a demo?
What Makes Remedly’s Revenue Cycle Management (RCM) Solution Different?
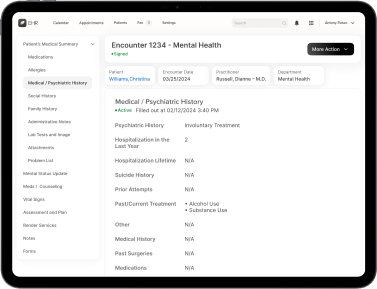
Our cloud-based medical billing software is a revenue cycle management service designed to suit medical practices of all sizes and at any stage of development. The software records every patient interaction beginning with initial registration, and it takes care of each financial interaction and securely stores all data.
This RCM healthcare service includes built-in reporting capability to provide analytics at the touch of a button. You can gain a comprehensive understanding of exactly what is performing well within your practice, and which areas could be improved. Think of Remedly as your practice’s very own CFO, making medical billing stress a thing of the past.

Our electronic medical billing software is designed to integrate with our EHR, allowing your practice to maintain accurate patient information, ensure data security, determine and achieve business goals, improve interactions, increase efficiency, and decrease billing inaccuracies, all while increasing profits. We work closely with our merchant services vendors to ensure transactions are frictionless and error-free. Remedly has a well-deserved reputation as a trusted partner with our vendors which, combined with our intuitive software, means claims are more likely to achieve maximum reimbursements. In collaboration with domain experts in claims management, Remedly identified and eliminated frequently-occurring bottlenecks during the insurance billing process from claim creation to submission and insurance payment through remittance disbursement, to ensure a smooth claim lifecycle. Our revenue cycle management solution makes it easy to track the status of any claim at any given time, allowing practitioners to focus more on their patients and spend less time investigating the status of claims.
How can our RCM healthcare software help to reduce denied claims and increase revenue?
This feature allows a provider to track claim initiation, the response to the claim, and the rationale behind claim denials. Providers can send accompanying notes alongside claims which improve communication, reduce misunderstandings, and minimizes the number of denials. Our claims scrubbing tool keeps the wheels turning to improve your claims acceptance rate. Insurers can respond with notes about the claim, keeping the dialogue open and all parties up-to-speed.
Remedly’s RCM billing software means providers can more easily collect payment from patients with outstanding balances and claim bills from insurers. In addition, our medical billing software logs all of these transactions for historical review.
Remedly’s AI Assistant uses machine learning to predict the acceptance or rejection of claims by clearinghouses and insurance companies before submitting them.
Full-Service and Self-Service
Based on size of practice, manpower and types of collections, you can either employ the Full-Service or Self-Service option. Full-Service is best suited for practices which prefer outsourcing their claims management. Self-Service , a.k.a. in-house billing, is optimal for clinics which have their own billers. The medical billing software price reflects the level of services you choose.