- Long SOAP Note Example
- Short SOAP Note Example
- SOAP Notes Structure
- Subjective
- Objective
- Assessment
- Plan
- Other Info
- Tips for Writing SOAP Notes
- Common Abbreviations
Table of Contents:
How do doctors organize all the information about their patients? Back in the 1950s, Lawrence Weed asked himself the same question and came up with a solution — the SOAP notes.
SOAP notes are a way for healthcare providers to document patient data more efficiently and consistently. Today, the C-CDA (Consolidated Clinical Document Architecture) has set out a standard format for SOAP notes with a wide range of sections. However, not all sections are needed for every note, so healthcare providers can choose the most relevant sections for their specialty.
This article provides examples of SOAP notes in both narrative and abbreviated formats, as well as a list of acceptable clinical documentation abbreviations.
NOTE: Abbreviations can improve efficiency but can be confusing if used incorrectly. The Joint Commission’s "Do Not Use" list and the Institute for Safe Medication Practices’ list of Error-Prone abbreviations are essential to maintaining clear and safe medical documentation.
Long SOAP Note Example
Subjective
- Chief Complaint
The patient states they have been "stressed out by daily life" and has had difficulty concentrating for over three months. - Medical History
The problem began around three months ago and has continued consistently, affecting the patient’s mental and cognitive functioning. Daily stressors primarily exacerbate the stress and concentration problems and seem to improve slightly with rest and relaxation. The patient notes that the intensity of the symptoms fluctuates throughout the day, often worsening during periods of high stress. They rate the severity of their symptoms as 7 out of 10, indicating a significant impact on their daily functioning.
Objective
The patient appeared mildly anxious during the session, but no acute physical abnormalities were observed. A cognitive assessment revealed moderate impairment in concentration and attention, consistent with the patient's complaints.
Assessment
The patient has moderate anxiety and difficulty concentrating due to chronic stress and a family history of anxiety and depression.
Plan
The patient will continue their current medication regimen and begin CBT. Follow-up appointments are scheduled, and referrals for stress management programs are made. The patient is also advised to engage in regular physical activity and mindfulness practices.
Short SOAP Note Example
Subjective
- CC
Pt. Is "stressed out by daily life" and has difficulty concentrating for over 3 mo.
- MH
Prob started 3 mo. ago, consistently affecting pt’s mental function, w/ sx worsening under stress and Sl. improving w/ rest. Pt rates severity as 7 out of 10.
Objective
During the session, pt. was mildly anxious, but 0 acute physical abnormalities observed.
Cognitive assessment → mod impairment in concentration and attention, consistent w/ pt's complaints.
Assessment
Pt. mod anxiety and difficulty concentrating b/c of chronic stress and FH of anxiety and depression.
Plan
Pt. cont current med regiment and begin CBT. F/U appt is scheduled and ref for stress management program.
Pt. is advised to engage in reg. physical activity and mindfulness practice.
SOAP Notes Structure
The SOAP notes structure organizes scattered patient data into a clear and cohesive health narrative. Recognizing the need for a structured but comprehensive approach to capturing health stories, an alliance of healthcare vendors, providers, and associations spearheaded an initiative to standardize medical documentation called The Health Story Project.
Although it’s no longer active, its impact on the health IT community has been significant. For example, it has seen extensive application in educating professionals on creating thorough electronic health records, setting the stage for today's advanced documentation practices.
The following sections highlight the basic information consistent with the SOAP Notes framework, as detailed in the HL7 CDA R2 Implementation Guide. We encourage you to regularly review the updated versions of this guide to get a more complete understanding and stay up to date.
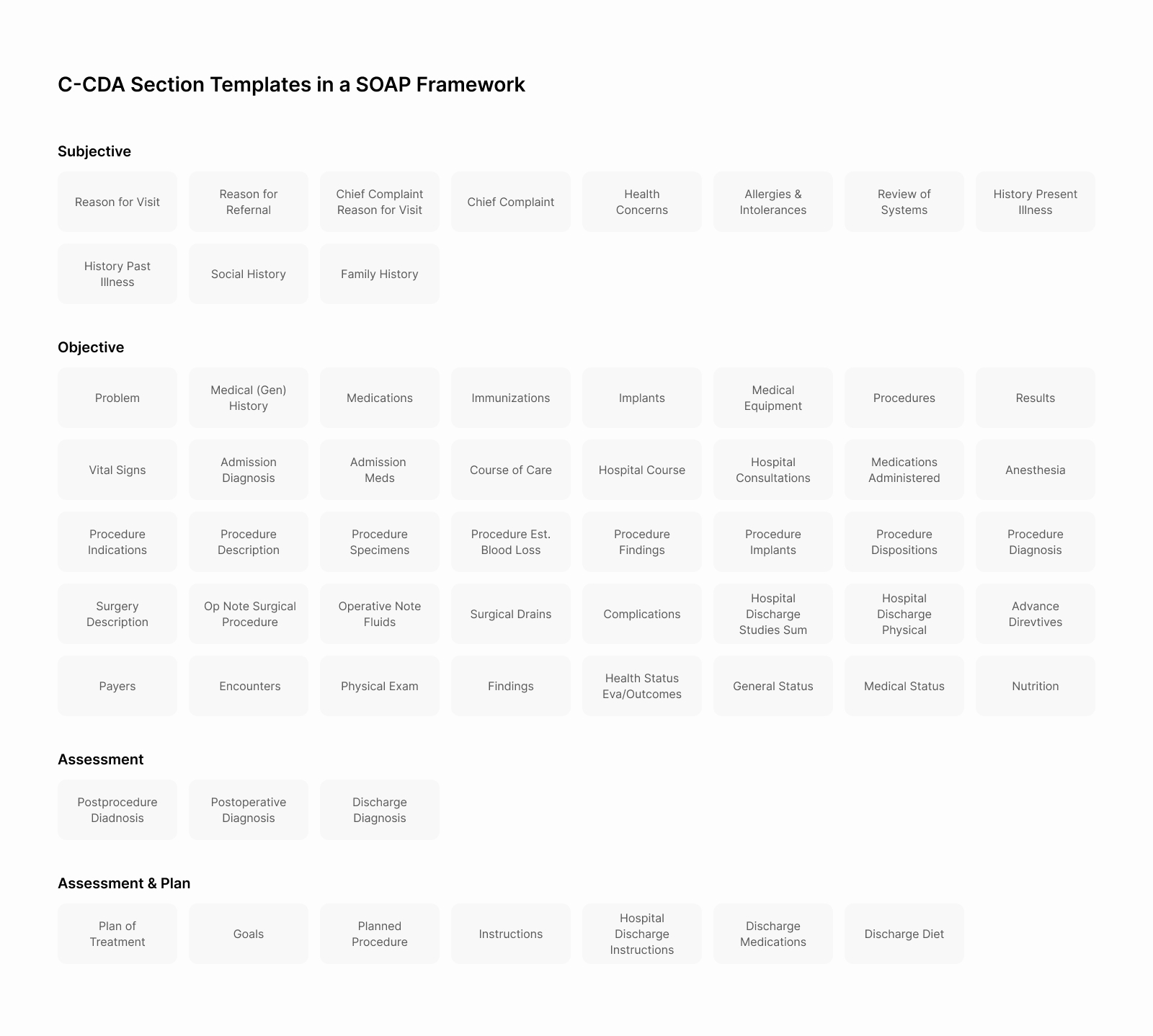
SOAP notes are made up of four major sections:
Subjective
The Subjective section provides a narration-style description of the patient's current condition. It encompasses the patient's experiences, views, and feelings, offering a crucial context for the Assessment and Plan sections. These patient-oriented data have to address specific key components, including but not limited to:
Reason for Visit and/or Chief Complaint
Depending on local policy, providers can submit these components separately or combined. The "Reason for Visit" reflects the doctor's perspective on why the patient seeks care, while the "Chief Complaint" summarizes the patient's account of their symptoms.
History of Present Illness
Physicians provide more details on the patient’s complaints in this sub-section, emphasizing the historical context. To ensure a complete outline, use the OLDCARTS acronym:
- Onset – When did the problem begin?
- Location – Where is it occurring?
- Duration – How long has the problem lasted?
- Characterization – How does the patient describe the problem?
- Alleviating/Aggravating factors – What factors make it better/worse?
- Radiation – Does it remain in one place or spread to other areas?
- Temporal factors – Does the problem vary in intensity throughout the day?
- Severity – On a scale from 1 (mild) to 10 (severe), how would the patient rate the intensity of their symptom?
Social History Section
This section covers social and demographic information that could affect the patient's physical, mental, or emotional well-being, such as smoking, pregnancy, employment, marital status, race, ethnicity, and religious affiliation.
Objective
The Objective section of the SOAP notes includes patient data collected through tests, measurements, and observations that provide quantifiable or categorizable results. This section can also include information specific to Procedure and Operative Notes and Inpatient Encounter Notes. Typically, the Objective section comprises the following components:
Objective Section
This subsection includes significant positive and negative test results, such as data from physical examination findings, a comprehensive review of body systems, and other relevant observations and measurements.
Problems Section
This section lists all relevant clinical problems, including current and historical issues, to reflect the patient's overall health status.
Medication Section
This is where clinicians document the patient's current medication regimen and relevant medication history. It can also detail the patient's prescription and dispensing history here to get a comprehensive overview.
Recording is essential for tracking and managing treatment. It allows for reviewing past prescriptions, making adjustments based on the patient's condition, and planning future steps. Proper recording helps monitor progress and make informed adjustments.
Results Section
The Results section presents the outcomes of observations generated by imaging, laboratories, and other procedures. This is where healthcare providers record notable findings, such as significant trends or abnormal values, which can help them fill in the Assessment and, ultimately, the Plan sections.
Assessment
The Assessment section, also known as "impression" or "diagnoses" outside of CDA, is a crucial component of the SOAP notes. It contains the clinician's conclusions and treatment guidance, combining Subjective and Objective data. Doctors can also write Procedural and Operative notes, as well as Inpatient Encounter Notes here.
This section includes some of the following components:
Assessment
In this subsection, sometimes called "Assessment and Plan," clinicians outline the conclusions and assumptions guiding the patient's treatment. Submitting the Assessment and Plan together or separately is possible depending on local policy requirements.
Postprocedure Diagnosis
When healthcare professionals make or confirm a diagnosis during medical procedures, they record it here. This information gives valuable insights into outcomes and helps guide future care decisions.
Clinicians use the Assessment information to create the Plan, the final part of the SOAP notes.
Plan
The Plan outlines the patient's goals and desired care outcomes and guides clinicians on the steps to follow during patient management. This section also incorporates elements specific to Procedure and Operative Notes and Inpatient Encounter Notes.
Key components of the Plan section include:
Advance Directives Section
This subsection contains vital information about the patient's healthcare preferences and legal arrangements, including healthcare proxies, living wills, CPR status, etc.
Plan of Treatment
Formerly known as the "Plan of Care," this subsection outlines pending orders, interventions, encounters, services, and procedures for the patient. It focuses exclusively on future, unfulfilled, or incomplete requests, covering all active, pending events of clinical significance to the patient's care.
The Plan section ensures continuity and consistency in treatment approaches by providing a clear roadmap for patient care.
In addition to the fundamental SOAP notes components, the SOAP Notes can include other data.
Other Info
SOAP notes can include additional sections that are not part of the main structure. These are:
Encounters Section
This section provides a detailed account of healthcare encounters relevant to the patient's current or past health status. Documenting these interactions can help clinicians gain valuable context about the patient's medical history and the continuity of care they've received. This information creates a clearer picture of the progression of conditions and the effectiveness of previous interventions.
Payers Section
The Payers section details the patient's financial arrangements for healthcare, including third-party insurance, self-pay options, and other guarantors. It also identifies who is responsible for the care costs, providing essential information for billing and administration. Physicians find all the contact and billing details for each payer here, as well as authorization details for referrals, therapies, procedures, or devices.
While these sections may not directly affect clinical decision-making, they are significant in ensuring seamless care delivery and proper administrative processes.
Recognizing that clinicians sometimes find writing SOAP notes challenging, we've prepared some recommendations to streamline the process. In addition to making the task easier, these tips will ensure that one’s notes are more manageable, accurate, and efficient.
Tips for Writing SOAP Notes
The importance of SOAP notes in the patient-physician interaction cannot be overemphasized. Despite the potential to vary their style format, all SOAP notes must include Subjective, Objective, Assessment, and Plan sections. These notes facilitate communication, as they can convey relevant information to other healthcare professionals, insurance companies, and legal practitioners.
We've compiled the following tips to help healthcare providers create clear and concise SOAP notes:
- Prioritize interaction and document later
The goal here is to focus on the patient during the visit. Take brief personal notes and then write formal SOAP notes in a readable format afterward. This approach ensures undivided attention during interaction with the patient and a more comprehensive documentation.
- Avoid delaying the paperwork
Document encounters immediately after the visit, ideally within 10 minutes, to ensure all necessary details are fresh in your mind. Prompt documentation reduces the risk of missing important information.
- Reduce unnecessary words
Short narratives are your friends when it comes to note-writing. Be concise while writing and document only what is most important. This approach saves time and provides more valuable information to other practitioners involved in the treatment process.
- Contextualize
Avoid fragmented and unrelated sentences. Present all information clearly and concisely, as it will eventually be linked and referenced to related content within and between practices.
- Be impartial
Provide specific, evidence-based information without being judgmental or presumptuous. Avoid making statements without supporting evidence to maintain objectivity.
- Avoid using pronouns
Improve clarity by identifying subjects using terms like "the client" or "this clinician" to avoid ambiguity. This practice ensures clear attribution of actions and observations.
- Note significant details
Try to include paraphrased statements, relevant quotes, patient-reported progress, and connections to the goals previously stated in the Subjective section. Depending on your specialty, note the client's level of attention, engagement, feedback from family or other providers, and any client testimonials that are considered significant.
While trying to get your SOAP notes in order, remember that the HIMSS Health Story Project states, "Clinical records must be complete, well-organized, easy to navigate, concise, logical, and adaptable to the needs of the user, shareable, readily available, and secure."
The SOAP notes must accurately capture and reflect the clinician's thought process, providing a comprehensive yet concise record of patient care. Now, let’s get to the most interesting part.
Common Abbreviations
To streamline the note-taking process, we've compiled an essential list of abbreviations for healthcare providers. Although this list isn’t exhaustive, it’s worth checking the "Do Not Use" list of abbreviations and the list of Error-Prone abbreviations from regulatory bodies.
Additionally, most healthcare facilities have their own list of approved abbreviations, so it is crucial to stick to one’s institution's guidelines to ensure clarity and patient safety in the documentation.
Download medical abbreviations

 Back
Back